About the issue
The HIV pandemic has had a serious effect on breastfeeding promotion and practice. When it was discovered that the virus could be passed from an HIV infected mother to her child through breastfeeding, many people became afraid, and efforts to promote exclusive breastfeeding and the Baby-Friendly Hospital Initiative slowed. People often assumed that all babies who were breastfed were likely to be infected – in fact only about 1 in 7 babies of HIV-positive mothers were infected this way, even when no precautions were taken to prevent transmission. Health services and agencies advised mothers to feed their babies artificially and in some situations they were given free formula, and there was concern about “spill-over” of artificial feeding to mothers who were HIV-negative.
Women who live in favourable socio-economic circumstances can afford enough formula, water, fuel and equipment to give reasonably safe artificial feeds, and it was accepted that for them, if they are HIV positive, this is usually the safest way to feed their babies. But it soon became apparent that for mothers without these advantages formula feeds were unsafe, and the risk to their babies of artificial feeding was greater than the risk of HIV transmission. For a number of years attempts were made to help mothers by counselling them about their infant feeding decision, and teaching them to feed their babies artificially in the safest way according to their circumstances. But it was difficult to give health workers enough training to counsel all the mothers in need in the best way. Many babies became ill, even though they were not infected with HIV. The dilemma for mothers about whether to breastfeed their babies or feed them artificially has continued for nearly two decades.
By 2006, it was known that HIV transmission occurred much less often with exclusive breastfeeding, and more often with mixed feeding with formula or early complementary foods. Mixed feeding is a very risky way to feed a baby, bringing both a greater likelihood of HIV transmission and an increased risk of death from other infections and malnutrition. A mother should either breastfeed exclusively, or formula feed exclusively. Exclusive breastfeeding is the first choice, and formula feeding should only be attempted if all the necessary conditions to do it safely are met.
By 2010, there were further important advances. It has now been shown that if a mother receives anti-retroviral drugs (ARVs, which are used to treat HIV), all the time that she is breastfeeding, transmission of HIV to the baby is largely prevented, and the number of infants who are infected falls very low.
These rapid advances in our knowledge have resulted in many changes in health policy, which have made necessary many changes in guidelines for health workers.
Exclusive breastfeeding has become once more the recommended way to feed all babies, whether their mothers are HIV infected or not. The Baby-Friendly Hospital Initiative can be confidently promoted once again.
There is now a need to make the new developments and policies widely known and understood through all sections of society. Many people are still confused, so it is important now to promote exclusive breastfeeding for the whole population, and to promote the use of ARV drugs for mothers who are HIV infected. Only those HIV positive mothers who have all the necessary facilities for safe formula feeding should avoid breastfeeding.
We hope that this website will help surfers to access the latest policy guidelines, so that they can be clear about the way forward.
Red Ribbon and the Golden Bow
 The Red Ribbon means the global response and solidarity with people living with HIV. The Golden bow means breastfeeding is the gold standard for infant feeding. Together it means responsiveness and support for women, mothers, girls and babies for survival, food security, better reproductive health, gender equity and community support. Wear the Red Ribbon and the Golden Bow now! To get one, click here
The Red Ribbon means the global response and solidarity with people living with HIV. The Golden bow means breastfeeding is the gold standard for infant feeding. Together it means responsiveness and support for women, mothers, girls and babies for survival, food security, better reproductive health, gender equity and community support. Wear the Red Ribbon and the Golden Bow now! To get one, click here
WABA World AIDS Day Statements
Click on the link below to read the full statement
HIV resource
Understanding International Policy on HIV and Breastfeeding: a comprehensive resource
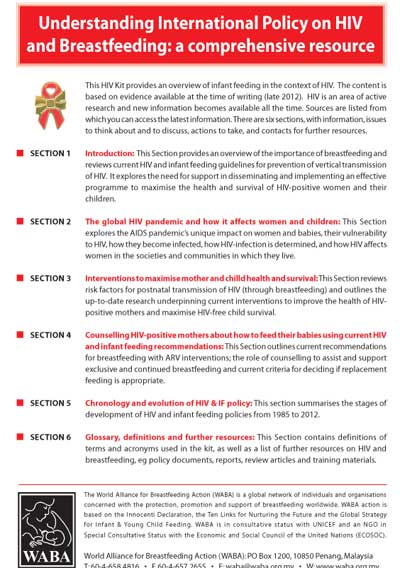 “Understanding International Policy on HIV and Breastfeeding: a comprehensive resource”
“Understanding International Policy on HIV and Breastfeeding: a comprehensive resource” is a resource which aims to clarify the confusion which has arisen during the last decade due to changing HIV and infant feeding guidance. The resource is intended for policy-makers, breastfeeding advocates, national breastfeeding committees, public health advocates, women’s health activists and others working in the community.
The resource also summarises up-to-date scientific evidence as at the end of 2012. Research emerging between WHO’s 2006 and 2010 guidance documents showed conclusively that maternal/infant ARV regimens during pregnancy and breastfeeding greatly reduce vertical transmission of HIV; and that exclusive and continued breastfeeding significantly improves overall HIV-free survival.
Resources, Useful Research and Links
Breastfeeding Gateway : HIV
 HIV/AIDS is not discriminatory. It could affect anybody, and babies are not spared from this risk. When a child is brought into the world, we wish the best for the child. However, sometimes, reality hits hard. There has been debate on the interventions HIV/AIDS is not discriminatory. It could affect anybody, and babies are not spared from this risk. When a child is brought into the world, we wish the best for the child. However, sometimes, reality hits hard. There has been debate on the interventions
WHO
Guidelines on HIV and infant feeding 2010. Principles and recommendations for infant feeding in the context of HIV and a summary of evidence.
 These guidelines were produced by the World Health Organization Department of Child and Adolescent Health and Development and HIV, in collaboration with UNAIDS, UNFPA and UNICEF. These guidelines were produced by the World Health Organization Department of Child and Adolescent Health and Development and HIV, in collaboration with UNAIDS, UNFPA and UNICEF.
UNICEF
UNICEF's Support to Free Infant Formula for Infants of HIV-Infected Mothers in Africa 2004
UNICEF began supporting Governments in providing services to HIV-infected mothers to prevent the transmission of HIV from mother to child (PMTCT) in 1998. Initially this support was to 11 countries in order to pilot the feasibility of PMTCT services, but more recently an increasing number of countries have started PMTCT activities or are planning to do so. As of December 2002 UNICEF had provided support to the planning and/or implementation of PMTCT in 54 countries. These projects support pregnant women with HIV testing and counseling, improved health care, anti-retroviral drugs, and counseling on infant feeding options.
Current Status Of Protection, Support And Promotion Of Breastfeeding In Four African Countries
The visits were conducted by Michael Latham, Professor of International Nutrition, Cornell University and Mrs. Pauline Kisanga, Regional Coordinator, IBFAN Africa. The following report highlights some interesting and disturbing facts about the current status of breastfeeding in the countries visited.
HIV-Positive - OK to Breast-feed
The scientific community accepted that there is reduced risk of breastfeeding compared to formula feeding for HIV positive mothers in Africa & Asia. Podcast interviewing South African pediatrician Hoosen Covadia, on the acceptance by the scientific community.
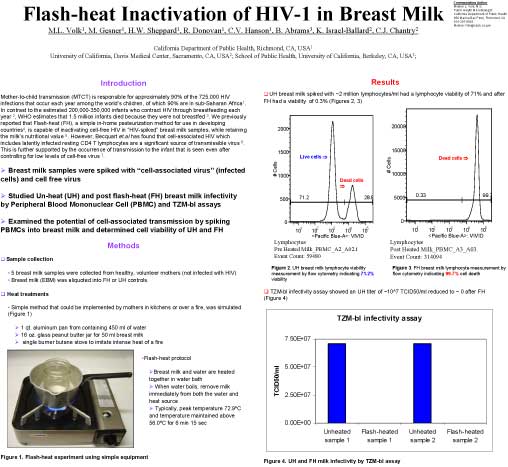
Flash-heated breastmilk can be utilized for "replacement feeding".
 Data suggest that Flash-heat, a simple home pasteurization method, is often an acceptable infant feeding option for HIV positive mothers in developing countries where access to safe infant formula is not a realistic choice. Data suggest that Flash-heat, a simple home pasteurization method, is often an acceptable infant feeding option for HIV positive mothers in developing countries where access to safe infant formula is not a realistic choice.
Flash-heat Inactivation of HIV-1 in breastmilk
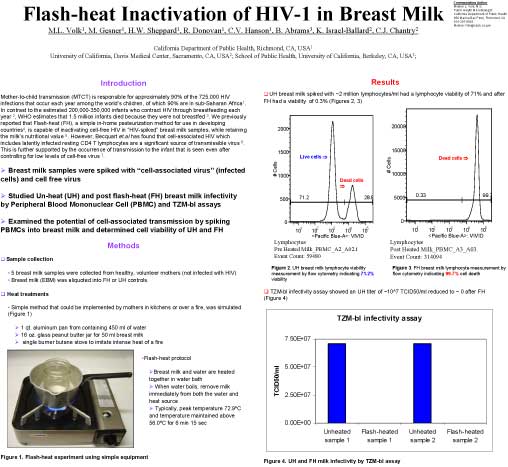 We previously reported that Flash-heat (FH), a simple in-home pasteurization method for use in developing countries4, is capable of inactivating cell-free HIV in “HIV-spiked” breastmilk samples, while retaining the milk’s nutritional value. However, Becquart et.al has found that cell-associated HIV which includes latently infected resting CD4 T lymphocytes are a significant source of transmissible virus. This is further supported by the occurrence of transmission to the infant that is seen even after controlling for low levels of cell-free virus We previously reported that Flash-heat (FH), a simple in-home pasteurization method for use in developing countries4, is capable of inactivating cell-free HIV in “HIV-spiked” breastmilk samples, while retaining the milk’s nutritional value. However, Becquart et.al has found that cell-associated HIV which includes latently infected resting CD4 T lymphocytes are a significant source of transmissible virus. This is further supported by the occurrence of transmission to the infant that is seen even after controlling for low levels of cell-free virus
back to top
|
Updates
|
|


 The Red Ribbon means the global response and solidarity with people living with HIV. The Golden bow means breastfeeding is the gold standard for infant feeding. Together it means responsiveness and support for women, mothers, girls and babies for survival, food security, better reproductive health, gender equity and community support. Wear the Red Ribbon and the Golden Bow now! To get one, click
The Red Ribbon means the global response and solidarity with people living with HIV. The Golden bow means breastfeeding is the gold standard for infant feeding. Together it means responsiveness and support for women, mothers, girls and babies for survival, food security, better reproductive health, gender equity and community support. Wear the Red Ribbon and the Golden Bow now! To get one, click  “Understanding International Policy on HIV and Breastfeeding: a comprehensive resource” is a resource which aims to clarify the confusion which has arisen during the last decade due to changing HIV and infant feeding guidance. The resource is intended for policy-makers, breastfeeding advocates, national breastfeeding committees, public health advocates, women’s health activists and others working in the community.
“Understanding International Policy on HIV and Breastfeeding: a comprehensive resource” is a resource which aims to clarify the confusion which has arisen during the last decade due to changing HIV and infant feeding guidance. The resource is intended for policy-makers, breastfeeding advocates, national breastfeeding committees, public health advocates, women’s health activists and others working in the community.